Abstract
Introduction: Despite being the prototypical indolent non-Hodgkin lymphoma, follicular lymphoma (FL) is a heterogeneous disease with a subset of patients experiencing early progression or histological transformation and poor overall survival. Upfront identification of these high-risk patients remains an area of unmet need. Interim positron emission tomography/computed tomography (iPET) is commonly used to identify suboptimal response while on therapy but data supporting this practice in FL are limited. We aimed to evaluate the prognostic impact of iPET response assessment using the Deauville 5-point scale (DS) in FL patients treated with frontline chemoimmunotherapy (CIT).
Methods: Patients with FL (grade 1-3A) who underwent iPET after 2-4 cycles of frontline CIT at a single academic center from 2008-2020 were identified. Patients treated with prior radiotherapy or rituximab monotherapy were excluded. Baseline, interim and end-of-treatment (EOT) PET scans were re-read by a nuclear medicine specialist using the DS. Progression-free survival (PFS) and overall survival (OS) were estimated with the Kaplan-Meier method and compared with the log-rank test. Cox proportional hazards model was used for multivariate analysis.
Results: 143 patients were included. The median age was 64 (range 28-86). Forty patients (28%) had grade 3A FL and 126 patients (88%) had stage 3-4 disease. FLIPI score was low for 20%, intermediate for 34% and high for 46% of patients. The CIT used were R-CVP (68%), BR (17%) or R-CHOP (15%) and 59% of patients received rituximab maintenance. Most iPETs (90%) were performed after 3-4 cycles. iPET DS was 1-2 for 59%, 3 for 13% and 4-5 for 28%. Six patients changed therapy based on progression on iPET; four of them had a confirmed histologic transformation. EOT PET was available for all other 137 patients with EOT DS of 1-2 for 72%, 3 for 4% and 4-5 for 24%.
During follow up, 63 patients (44%) relapsed or progressed, including 14 patients (10%) with a biopsy-proven transformation in aggressive lymphoma, and 25 patients (17%) died. Progressive lymphoma was the most common cause of death (n=15; 10 of these were from histologic transformation), followed by other malignancy (n=5, including one case of treatment-related AML), cardiovascular cause (n=3) and one treatment-related mortality (liver failure related to hepatitis B reactivation).
With a median follow up of 67 months, the median PFS was 70 months (95% CI 22- 119) and median OS was not reach for the entire cohort with a 2-yr PFS of 70% (95% CI 62-77) and 5-yr OS of 85% (95% CI 77-90).
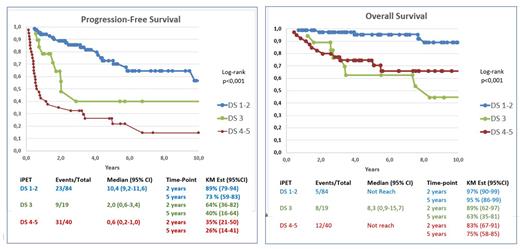
IPET was a significant predictor of PFS and OS with a 2-yr PFS 89% vs 64% vs 35% (p=<0,001) and 5-yr OS of 95% vs 63% vs 75% (p<0,001) for DS 1-2 vs 3 vs 4-5 respectively (figure 1)
EOT PET was also a significant predictor of PFS and OS with a 2-yr PFS of 92% vs 80% vs 18% (p<0,001) and a 5-yr OS of 94% vs 75% vs 65% (p<0,001) for DS 1-2 vs 3 vs 4-5 respectively.
In the multivariate analysis, adjusting for FLIPI and histological grade at diagnosis, iPET DS of 4-5 was an independent factor for worse PFS (HR 5,1 95% CI 2,9-9,1) and OS (HR 6,6 95% CI 2,3-19,3). Patients with iPET DS 3 had a non-significant worse PFS (HR 1,7 95% CI 0,8-3,8) but a significant worse OS (HR 9 95%CI 2,8-29,5) than those with iPET DS1-2. However, most deaths in patients with iPET DS 3 were not related to the underlying lymphoma.
Conclusion: In this cohort of FL patients treated with frontline CIT, an iPET DS of 4-5 was predictive of inferior PFS and OS, independently of FLIPI and initial histological grade. A DS of 3 was seen in few patients and had lower predictive value. Whether outcomes can be improved by response-adapted therapy remains to be determined and studies are needed to inform optimal care in this setting.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal